 Vermox Myths Debunked: Separating Facts from Fiction
Vermox Myths Debunked: Separating Facts from Fiction
Vermox Safety: Separating Risk from Reality
Personal stories make safety concerns feel urgent, but context matters; Vermox has decades of clinical use and well-known risk profiles.
| Risk | Reality |
|---|---|
| Common mild | Brief gastrointestinal upset |
Serious adverse events are rare and usually linked to preexisting liver or blood conditions; monitoring and proper dosing reduce risk and alternatives exist for specific infections. Treatment choice often depends on parasite type and patient history.
Discuss concerns with clinicians, weigh benefits against rare harms, and remember that evidence guides practical decisions. Regular follow-up and lab checks help personalize safe use with consent.
Does Vermox Kill All Parasites Instantly?

A patient remembers the panic of a positive stool test, imagining worms disappearing overnight. Reality is different: vermox paralyses parasites, preventing them from absorbing glucose so they die over days and are expelled. Immediate disappearance on symptoms is uncommon. Symptoms may linger while the body clears debris, so patience is required and follow-up tests help.
Effectiveness depends on parasite type: pinworms often respond to a single dose, while tapeworms or roundworms may need longer or different drugs. Lab confirmation and follow-up can show clearance rather than instant cure.
Clinicians balance speed with safety, often repeating doses or treating household contacts to prevent reinfection. Understanding how vermox works helps set realistic expectations and reduces unnecessary worry.
Common Side Effects Versus Rare Serious Reactions
Many people start treatment worried, imagining worst-case outcomes; in reality vermox commonly causes mild, short-lived effects such as nausea, abdominal discomfort, or headache, which often resolve within a few days without additional intervention or treatment.
Serious adverse events are uncommon but real: allergic reactions with rash or breathing difficulty, and rare hepatotoxicity have been reported. Prompt reporting of unusual symptoms helps clinicians assess risk and stop drug if deemed necessary.
For most users no lab monitoring is needed, but prolonged or repeated courses warrant liver enzyme checks. Patients with existing hepatic disease or taking hepatotoxic drugs should consult their clinician to weigh benefits, plan monitoring.
Overall, serious reactions to vermox are rare; most discomfort is transient. Follow prescribing instructions, avoid self-medicating, and seek medical attention if you experience high fever, jaundice, severe abdominal pain, or signs of an allergic reaction.
Vermox during Pregnancy: What Evidence Shows

When a pregnant person learns they have intestinal worms, alarm bells ring; questions about safety and treatment flood in. Fortunately, real-world evidence about vermox is more nuanced than panic suggests.
Animal studies showed adverse effects at very high doses, but human research is limited and has not demonstrated a clear increase in birth defects with standard antiparasitic dosing. Large public-health programs and WHO guidance support single-dose deworming after the first trimester in endemic areas to protect maternal health and fetal nutrition.
Clinicians weigh risks and benefits individually: avoid elective treatment in early pregnancy when possible, reserve therapy for confirmed infections or when maternal anemia is present, and always discuss options with a provider. Shared decision-making, accurate diagnosis, and appropriate timing reduce unnecessary fear while protecting mother and baby. Recent reviews urge reporting outcomes to improve evidence for better future guidance.
Over-the-counter Use: When Prescription Is Necessary
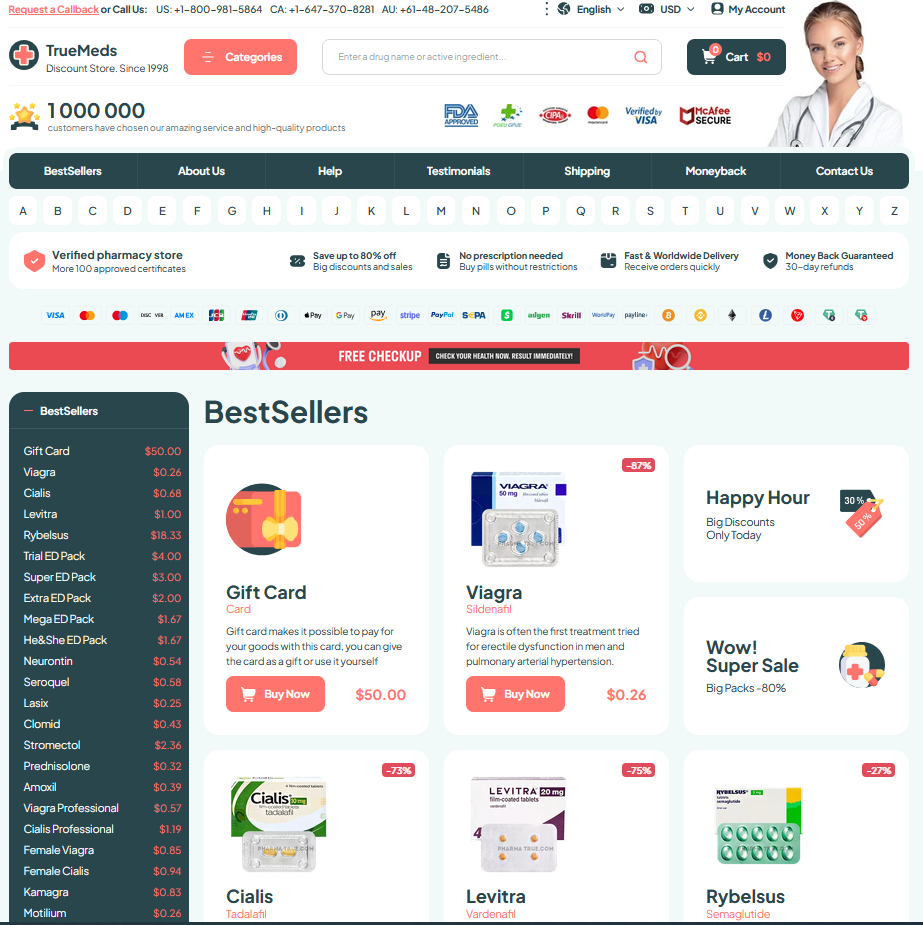
I remember the first time a friend asked whether she could buy vermox at a pharmacy without a doctor. The answer is not purely legal or practical; it depends on diagnosis, local regulations, and the parasite involved. And safe sourcing matters.
Pharmacies may sell generic antihelminthics OTC in some countries, but treating based on symptoms alone risks missing different organisms requiring prescription regimens.
| OTC? | When prescription needed |
|---|
When in doubt, seek testing rather than self-medicating; appropriate use of vermox is safest when guided by diagnosis and local professional advice. Stay informed, stay safe.
Dosage Myths: Single Dose Versus Repeated Courses
Many people imagine a single pill as a magic bullet, but reality is more nuanced. Vermox (mebendazole) often clears common intestinal worms with a short course, yet the parasite type and life cycle determine treatment length. Clinicians tailor regimens to ensure eggs and immature stages are targeted.
For some infections a one-day dose suffices; for others repeated courses separated by two to three weeks are recommended to catch newly hatched larvae. Ignoring timing can lead to apparent treatment failure even when the drug is effective, so follow-up and stool checks matter.
Patients should discuss history, exposures and concerns with their provider; blanket assumptions about single versus repeated dosing can cause unnecessary retreatment or under-treatment. Clear instructions, awareness of reinfection risks and adherence to the prescribed schedule improve outcomes and reduce myths about “instant cure” expectations and encourage appropriate diagnostic testing.

